What Is Anal Pain and When Should You See a Doctor?
Anal pain is a common symptom that affects individuals of all ages. It may present as either acute or chronic discomfort, felt in the anus, rectum, or surrounding area. The pain can occur suddenly or develop gradually over time. It is often accompanied by other symptoms such as itching, bleeding, difficulty with bowel movements, or a persistent feeling of pressure.
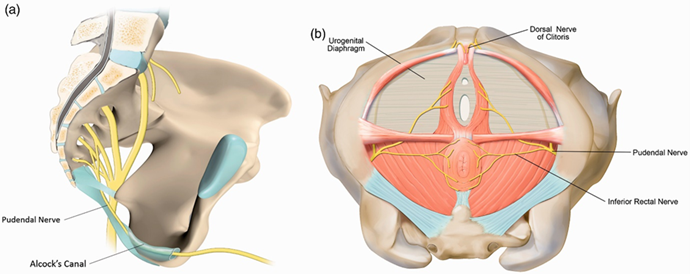
There are various causes behind anal pain. The most common include hemorrhoids, anal fissures, abscesses, fistulas, or impacted stool. However, in some cases, the pain may be due to less common causes such as nerve inflammation or pelvic floor muscle spasms.
This highlights the importance of proper diagnosis. Relying solely on symptoms is not sufficient—clinical examination is essential, and in more complex cases, further testing such as MRI scans may be required.
In Dubai, Dr. Daad Al-Taani is one of the leading specialists in diagnosing and treating anal and rectal conditions. With extensive experience, she provides accurate diagnoses and effective treatments tailored to each patient’s needs. Her clinic offers a wide range of treatment options, including medications, physical therapy, and surgical procedures when necessary.
Dr. Daad emphasizes the importance of not ignoring anal pain, especially if it persists for several days or is accompanied by bleeding or discharge. Early diagnosis can help prevent complications and reduce the need for surgical intervention.
In mild cases, pain relief may be achieved through simple methods such as warm sitz baths or dietary adjustments. However, in more serious conditions, medical intervention is required to treat the underlying cause.
This article explores the main causes of anal pain, associated symptoms, and how to accurately diagnose the condition. We also highlight the advanced treatments available at Dr. Daad Al-Taani’s clinic to help you regain your comfort and improve your quality of life.
📺 Follow Dr. Daad Al-Taani’s interviews and medical advice on our YouTube channel for valuable health insights.